Black gay community concerned monkeypox response is inadequate
In July, a 35-year-old Black man from the Washington, D.C. area went from experiencing Covid-like symptoms to watching his body be overtaken by the aggravating, blistering boils of monkeypox. And yet, as he endured the agony and uncertainty that came with the disease, he said he had other, more pressing concerns.
The man, who asked to remain anonymous because of concerns related to the stigma associated with the disease, said he was alarmed by how difficult it was to find information on monkeypox and his doctor’s seeming dismissal of his concerns about his symptoms.
He said his case is an example of the concerning public health response to monkeypox, and, for the Black population in particular, follows a historical pattern of medical malfeasance and shortcomings.
The man said when he visited urgent care in early July, the doctor didn’t appear to take him seriously. “I asked if she was up on the latest CDC guidelines on monkeypox and she wasn’t,” he recalled. “So, she had to call the CDC to even get approval to administer me a test. She went on about how it would take an hour of paperwork and other stuff, so most doctors weren’t excited about giving the tests.”
The man, who is gay, said, “it was like a repeat performance” of some of the issues that came with the Covid pandemic, when Black people in many parts of the country had less access to treatment and vaccines, according to the Centers for Disease Control and Prevention.
Now with monkeypox, health care officials face the challenge of effectively communicating information about the spread of the outbreak without stigmatizing gay men. Public health officials interviewed by NBC News said managing that balance is critical to gaining public confidence to offset the intense mistrust of the medical establishment in the Black community. The poor response by health officials, the disparities in the vaccine rollout and the stigma associated with monkeypox have contributed to men questioning how the virus is spread — despite the data, experts say.
Data from the CDC found that, through July 22, 99% of cases were among men, 94% of whom reported recent sexual contact with males. The World Health Organization added that 98.7% of confirmed cases globally are in males, with 97.2% of those men reporting that they had sex with other men.
Black men across the country have been hit especially hard by the outbreak. Although Blacks make up roughly 12% of the population, they make up 38% of the most recent monkeypox cases, according to the CDC. In Atlanta, 71% of people with the infection, which can cause painful and irritating skin lesions, are Black men who have sex with men and about two-thirds of those men have HIV, according to the Georgia Health Department.
In North Carolina, one of the few states reporting on the monkeypox spread, 70% of those infected are Black men, with nearly all of the cases affecting men who have sex with men. However, only 24% of the vaccines in the state have gone to Black North Carolinians.
Those numbers worry Black gay men, as well as public health experts like Dr. Jayne Morgan, director of Piedmont HealthCare in Atlanta who hosts educational podcasts on monkeypox. She said the messaging has to be clear about who is at risk of contracting monkeypox and what preventive measures are available, all while being careful not to stigmatize specific groups of people.
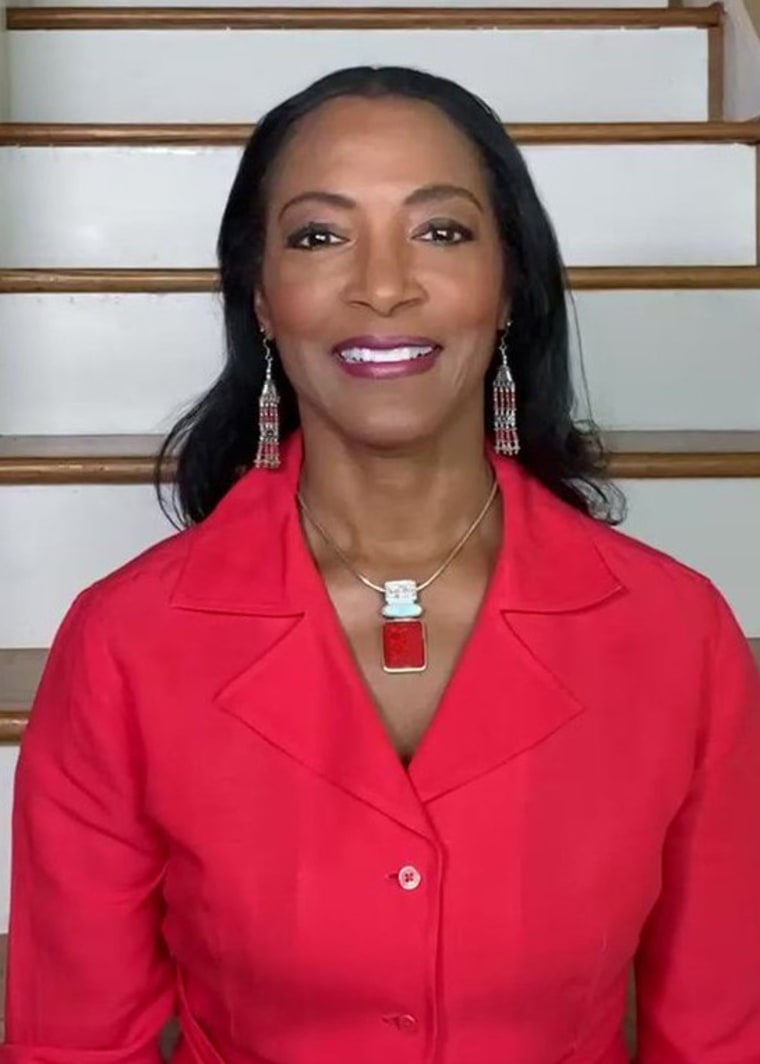
“We have the tools and enough information to stem this tide,” Dr. Morgan told NBC News. “Public health, like Covid, is about behavior. Monkeypox is being driven by behavior. And so behavior can also drive it in the opposite direction also.”
Health care experts believe that sex between men — both anal and oral intercourse — is likely the main driver of global monkeypox transmission. The skin contact that comes with sex, these experts say, is probably much less of a risk factor, citing studies published in peer-reviewed journals, as well as reports from national, regional and global health authorities, as previously reported by NBC News.
The statistics, misinformation and mistakes in the vaccine rollouthave Black gay men worried they could be seeing a repeat of the response and stigma that came with the HIV/AIDS epidemic of the 1980s.
The 35-year-old D.C. resident, who no longer has monkeypox symptoms, called it “dangerous.”
David J. Johns, the executive director of the National Black Justice Coalition, a civil rights organization committed to empowering the Black LGBTQ community and people living with HIV/AIDS, said the attention monkeypox is receiving now is happening only because non-Black people are also impacted.
“The sad reality is that monkeypox isn’t new,” Johns said, adding that it has existed in Africa since the 1970s. “But because privileged white men from Western societies — in particular America — are now being impacted by something that otherwise only impacted disposable Africans, there is a now shift in the way that people are thinking about and talking about and are responding to a virus that has been impacting people for a lot longer than we otherwise want to acknowledge.”
Get the Morning Rundown
Get a head start on the morning’s top stories.SIGN UPTHIS SITE IS PROTECTED BY RECAPTCHA PRIVACY POLICY | TERMS OF SERVICE
Difficulty in being diagnosed and treated
The man from the D.C. area said that after a weekend of activities and attending “a crowded party” on July 10, he woke up the next day, “not feeling my best.” He was fatigued and had a fever of 102 and had trouble focusing. He left work early, believing he had contracted Covid.
Recommended

U.S. NEWSExplosion at Colorado apartment building leaves hundreds displaced

U.K. ROYALSCharles proclaimed King of Scotland, Wales and Northern Ireland, queen’s coffin arrives in Edinburgh
He took a home test that came back negative. A test at urgent care confirmed he did not have the coronavirus. His fever eventually broke but he had a throbbing headache for days. And he said he experienced “rectal discomfort” and his blood pressure was elevated. Several days later, he began to feel better — but he noticed bumps on his face and arms.
After some resistance, the doctor finally swabbed the blisters on his face and wrists and sent him home with 800 milligrams of ibuprofen and a prescription for his anal pain. At his residence, he said he isolated himself in the attic. In the morning, he woke up to extreme throat soreness. He returned to urgent care, where the doctor again had to call the CDC to see how to treat him since he had been tested positive for monkeypox.
The physician was advised by the CDC to administer an antibiotic shot, which alleviated some of the throat pain. Meanwhile, the sores spread to other parts of his body — arms, legs, in particular.
But “it was kind of shocking,” he said, that his issues were not immediately addressed. He added he was given eight different numbers to call for assistance. “They dragged their feet the entire time.”
The man said he gave a list of the friends he had been in close contact with to the health department for contact tracing. He had already advised them to seek medical attention by the time the health department contacted them two weeks later. “And when they finally got someone, they were basically forced to say they had sex in order to get the vaccine,” he added, noting that his friends felt pressured to say they had sexual contact with him — even when some didn’t — in order to get immediate attention from health care professionals.
“When we talk about high-risk communities, we’re really talking about people who are sort of disaffected from the health care system,” Morgan said. “Stigma and discrimination for people in the LBGTQ community are already very high. And then if you add the Black race on top of that, and you have in monkeypox the same as we did with Covid — the black population is always the most vulnerable because we have the least resources, the least outreach and the most discrimination and stigma.”
In Los Angeles earlier in July, another Black man who also asked to remain anonymous because of the stigma associated with having the virus, outlined nearly identical concerns as the man in metro D.C. He, too, said he believed he didn’t contract the disease through sex. When symptoms occurred, he said he had difficulty finding a place that tested for monkeypox. And when he did locate a health center in downtown Los Angeles, the staff was “suited and booted as if I had a contagion,” he said, referring to the protective gear they wore.
Meanwhile, the disparity in those who have contracted monkeypox and those who have access to vaccines is glaring. While Black people account for about a third of monkeypox cases in the U.S., about 10% of vaccines have been administered to the group, according to the CDC.
The vaccine distribution disparities come as Dr. Rochelle Walensky, the head of the CDC, acknowledged that the agency must make drastic changes to respond better and faster to public health emergencies, following missteps during the Covid pandemic.
“We have learned less than nothing from Covid,” Stella Safo, a primary care physician at Mount Sinai who specializes in HIV treatment and is the founder of Just Equity for Health, told STAT News. “We’ve gone backwards.”

Dr. Tyeese Gaines, a physician who practices emergency medicine in Illinois and New Jersey, said the more than two years of being on alert from the coronavirus pandemic has created “panic fatigue,” exasperating people to the point where they are less apt to protect themselves against monkeypox.
“We needed to tell people the reality of Covid-19,” Gaines said. “But eventually people just don’t want to hear it anymore. Some people say: ‘Oh, wow, there’s another scary virus. Let me be safer.’ But there’s still a subset of people whose response to fear is not to become more conservative or to follow whatever the rules are, but actually to act like it doesn’t exist and do the opposite.”